Diabetic Retinopathy
Diabetic retinopathy is a vision impairing eye disease caused by diabetes-related damage to blood vessels in the retina. To learn more about diabetic retinopathy and its treatment, we encourage you to explore the sections provided below, or simply contact our practice today to book an appointment.
- What Is Diabetic Retinopathy?
- Diabetic Retinopathy Symptoms
- Diabetic Retinopathy Stages
- Diabetic Retinopathy Diagnosis
- Diabetic Retinopathy Treatment
- Diabetic Retinopathy Prevention
- Diabetic Retinopathy Causes
- Diabetic Retinopathy Risks
What Is Diabetic Retinopathy?
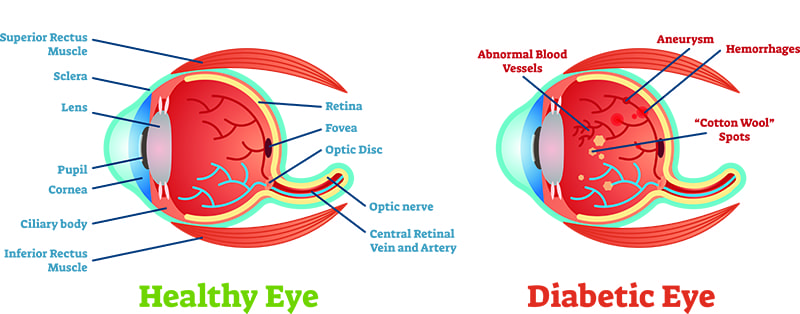
When blood sugar levels are poorly controlled in those who have diabetes, retinal blood vessels can progressively swell and leak, leading to gradual vision deterioration. This may begin as slight haziness or blurriness, but depending on the progression of the condition, it can advance to the presence of obstructive “floaters” and eventually to total blindness. In fact, diabetic retinopathy is the top cause of blindness among adults in the United States today.
Dr. Tory Prestera and Dr. Howard Guan are dedicated to helping patients with diabetes maintain their eye health. They regularly check for signs of diabetic retinopathy—a common condition that can lead to vision loss if not treated. Both doctors are skilled in providing effective treatments to prevent or manage vision deterioration from this condition. With a compassionate approach, they meet the unique needs of our diverse patient community, including the many Hispanic families we proudly serve. Dr. Prestera and Dr. Guan are committed to ensuring that every patient receives personalized and attentive care.
What Are the Symptoms of Diabetic Retinopathy?
Symptoms of diabetic retinopathy generally do not manifest during the initial stages of the disease, which is why regular eye examinations are crucial to detecting the condition early on. Once diabetic retinopathy has progressed, however, some signs may include:
- Blurry or hazy vision
- Double vision
- Floating spots or streaks (floaters)
- Blank or dark areas of vision
- Muted colors
- Fluctuation or deterioration of vision
- Partial or complete blindness
In most cases, these symptoms affect both eyes as opposed to just one.
What Are the Different Stages of Diabetic Retinopathy?
There are four stages of diabetic retinopathy:
- Mild Non-Proliferative Diabetic Retinopathy – In this first stage, the retinal blood vessels have tiny bulges (microaneurysms) that can cause small amounts of blood to leak into the retinas. It is likely that no symptoms are noticeable at this point.
- Moderate Non-Proliferative Diabetic Retinopathy – In this second stage, the blood vessels have swollen and often do not provide sufficient nourishment to the retina, which can cause physical retinal changes. Diabetic macular edema (DME) can also occur at this stage, which is when blood and other fluids accumulate in the macula—the part of the retina responsible for central vision. DME is the top cause of vision loss in individuals with diabetic retinopathy, and its occurrence becomes increasingly more likely as the disease progresses.
- Severe Non-Proliferative Diabetic Retinopathy – In this third stage, a significant number of retinal blood vessels become blocked, restricting critical blood flow to the retinas. This causes scar tissue to form and the retinas to signal for new blood vessels to be made. Once this stage is reached, treatment may be able to prevent further vision impairment, but any vision loss already incurred is likely permanent.
- Proliferative Diabetic Retinopathy – In this final stage, new blood vessels grow in the retina, which is known as neovascularization. Unfortunately, these recently developed vessels are often weak and abnormal, causing them to leak and bleed to the point that vision can be partially or fully lost. In addition, scar tissue can form, which may cause retinal detachment, glaucoma, and further contribute to partial or total vision loss.
How Is Diabetic Retinopathy Treated?
The treatment of diabetic retinopathy at Prestera Eye Medical Group will depend on the stage of the disease and the area of the retina that is impacted. The most important aspect is working with your primary care doctor to maintain control of your blood glucose. During the earlier stages of diabetic retinopathy, Dr. Prestera or Dr. Guan will likely simply monitor your condition on a regular basis to keep track of its advancement and be proactive about detecting potential diabetic macular edema (DME) as promptly as possible.
Should DME eventually occur—or if your diabetic retinopathy reaches the latter stages in which vision loss is often inevitable without intervention—Dr. Prestera or Dr. Guan can utilize intravitreal injections, retinal laser therapy, or a combination of both treatments to help prevent vision damage. Intravitreal injections involve injecting medication into the eye to prevent abnormal blood vessels from growing, and a retinal laser can be used to seal or eliminate blood vessels that are leaking, as well as get rid of scar tissue that has formed. Both of these treatment methods can be performed right here in our office, and they have proved to be highly effective in managing diabetic retinopathy and preventing permanent vision loss.
What Are Some Diabetic Retinopathy Prevention Tips?
Potential ways to avoid diabetic retinopathy mostly revolve around managing one’s diabetes. It’s important to note that while treatment for diabetic retinopathy is possible and can be successful at slowing the progression of the condition to a halt, there is not a definitive cure. Possible ways for those with diabetes to avoid diabetic retinopathy include: monitoring your blood sugar; safely and accurately managing your diabetes; eating a balanced and healthy diet that avoids salty, fatty, and sugary foods; maintaining an ideal weight; and exercising on a regular basis.
What Causes Diabetic Retinopathy?
Those who have been diagnosed with diabetes run the risk of developing diabetic retinopathy over time. Diabetic retinopathy appears in patients when blood vessels in the retina are blocked by having an abundance of sugar in one’s blood. When the retina attempts to naturally counteract this condition, newer, underdeveloped blood vessels are created that are more prone to leaking. This phenomenon can lead to impaired vision and even vision loss.
How Is Diabetic Retinopathy Diagnosed?
Diabetic retinopathy can typically be identified through techniques utilized in a comprehensive eye exam. The process may include different testing approaches, such as:
- Visual acuity test – This measures how well you can read a series of letters to determine the extent of vision loss and any damage to central vision.
- Dilated eye exam – This technique involves droplets placed in the eyes to widen the pupils, making it easier to examine the retina and optic nerve for possible damage.
- Optical Coherence Tomography (OCT) – An OCT is a non-invasive test that utilizes light waves to take pictures of the retina. This makes it possible for eye care professionals to measure retina layers and detect any potential retinal swelling.
- Fundus photography – This approach utilizes a specialized fundus camera to take a detailed image of the retina, blood vessels, macula, and other components of the eye. The term “fundus” refers to the posterior area on the inside of the eye.
- Fluorescein angiography – A fluorescein angiography eye exam involves special dye and a camera to check the circulation in the retina.
Who Is at Risk of Developing Diabetic Retinopathy?
Susceptibility for developing diabetic retinopathy is primarily linked to how long a person has had diabetes and how they have managed their condition. While instances of people who develop diabetic retinopathy slightly differ with each case, there are general risk factors that may lead to the development of this condition. Common risk factors for individuals with diabetes that can lead to diabetic retinopathy include: a long history of diabetes, improper management of one’s diabetes, high blood pressure or high cholesterol, frequent and long use of tobacco products, and becoming pregnant.
Contact Prestera Eye Medical Group
For more information about diabetic retinopathy, or if you are interested in screening and/or treatment for this vision condition, please do not hesitate to contact us online or by telephone today to book an appointment.